Good Communication Can Help Prevent Harmful Mistakes with Medicines!
2013-10-29
Everyone experiences communication problems at one time or another. Maybe you've missed a meeting because you weren't told that the location had been changed. Or perhaps you've bought the wrong size or brand of an item at the supermarket because you didn't get enough information from the person who asked you to pick it up. Most communication mistakes cause nothing more than an inconvenience. But when it comes to medicines, a lapse in communication could lead to a mistake that could in turn cause serious harm.
Here is an example of an incident involving a communication breakdown that was reported to SafeMedicationUse.ca. A consumer was taking a medicine called ramipril to control high blood pressure. This medicine comes in several different strengths. The consumer had been taking two of the 10 mg capsules every day, for a total daily dose of 20 mg. However, the doctor thought the consumer was taking two of the 2.5 mg capsules, for a total daily dose of 5 mg. The consumer's blood pressure was still a bit too high, and the doctor instructed her to increase the dose to 3 or 4 capsules a day.1 Using the 2.5 mg capsules, the total daily dose would have been 7.5 mg to 10 mg. However, because the consumer used the 10 mg capsules she had on hand, she took 4 times the amount of ramipril that the doctor had intended! Eventually, a family member realized what had happened. The family had some difficulties sorting out the mix-up with the doctor's office and the pharmacy, but fortunately no harm was reported.
-
-
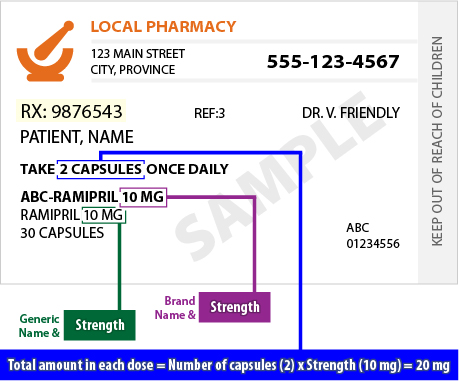
Figure 1 - Example of a Prescription Label *
*Example only, not all prescription medicine labels will appear exactly as shown
SafeMedicationUse.ca has the following suggestions for preventing communication problems with your medicines:
- Keep a list of all your medicines and how to take them. Be sure to update your list whenever there is a change in any of your medicines. Always show the list to healthcare providers when you receive care.
- Know the strength per unit of each medicine you are taking or using, the total amount to be taken for each dose and how many times a day you take it. The dose and strength are often expressed in grams, milligrams, micrograms, or units (see Figure 1). It is important to know this information for all forms of your medicines (for example, patches, liquids, creams, drops, injections, and inhalers, as well as tablets and capsules). Document this information on your list of medicines.
- If you are speaking about your medicines with a healthcare provider by telephone, be sure to refer to your list of medicines or your prescription bottles for details. Don't rely on memory!
- If you are instructed to adjust the dose of a medicine according to your symptoms, ask about the maximum dose that you can safely take at any one time. You should also know the maximum total amount that you can safely take in one day. This is called the "maximum daily dose".
- If a healthcare provider instructs you to change the way you are taking a medicine, be sure to get the new instructions in writing. You can ask your healthcare provider to help you make the necessary changes on your list of medicines.
- Be sure to update your pharmacy any time there is a change to the way you take a medicine. If your doctor writes a new prescription for a medicine that you are already taking, bring it to your pharmacy right away, even if you still have a supply of the medicine. This is especially important if the dose or instructions have changed and will ensure that your records at the pharmacy are up to date. It will also give you an opportunity to ask the pharmacist any questions you may have about the changes.
For more information, read our article on keeping a list of your medicines.
|
Tips for Healthcare Practitioners
The following steps can help prevent communication problems when the dose or dosing schedule of a current medicine is adjusted:
- Encourage patients to bring prescription vials and lists of medicines with them when receiving health care.
- Before making any changes to prescriptions, verify the current medication strength and directions for all medications against the patient's list of medicines and prescription vials.
- Review dose changes with patients to ensure they understand the new instructions.
- Provide patients with written instructions about the changes in dose or dosing schedule. This should ideally be done by providing a new prescription, even if the patient already has a supply of the medicine.
- Ensure that changes are communicated to other healthcare providers. Encourage patients to update their pharmacy about any changes to the way they are taking their medicines, even if a refill is not required. Consider faxing an "information only" copy of the prescription to the pharmacy.
- Assist patients to update lists of medicines.
|
1. Editor's Note: This report also raised concerns about lack of clarity in the dosing instructions, with regard to the number of capsules the consumer was supposed to take each day. We don't have all the details about the case, and the consumer may have received specific instructions about when to increase the dose from three capsules per day to four capsules. However, this situation reinforces the need for clear communication and monitoring when doses are being adjusted.
|

